Massachusetts Community Behavioral Health Center (CBHC) Resource Hub
About the CBHC Program
CBHCs are hubs of coordinated and integrated mental health and substance use disorder treatment for MassHealth members of all ages, providing routine and urgent outpatient services, crisis services for adults and youth, and community crisis stabilization services for adults and youth. Read the program procurement here.
About eHana
For the past 22 years eHana has delivered innovative Health IT software solutions, serving over fifty Massachusetts nonprofit providers. We are proud to be part of a caring and committed community that makes a difference in the lives on individuals, children and families impacted by behavioral health and substance use disorders. Learn more about eHana.
eHana CBHC Mailing List
Enter your email address below to sign up for eHana’s CBHC mailing list.
eHana Supports CBHCs
eHana partner organizations may use the information below in support of sections XIV.E.1.c.iii and XIII.F.5 of the CBHC RFP.
eHana has more experience and expertise than any other Health IT vendor in supporting Massachusetts Medicaid behavioral health providers adapting to meet the needs of the Roadmap for Behavioral Health Reform
The company’s extensive experience includes providing core technology to numerous Outpatient, ESP/MCI, and CCS programs, as well as 23 of the 27 MassHealth Community Partners (CP) and several Community Service Agencies (CSA)
eHana has over 15 years of experience working specifically with Massachusetts state agencies, payers, and other stakeholders, continuously and responsively adapting its technology for Massachusetts’ unique regulatory and payment needs
eHana’s core technology platform is designed to be extremely user-friendly, and is real-world validated to support multi-service patient records, care team collaboration, health data interoperability, and quality reporting analytics
Summary of eHana’s experience
eHana provides a certified Electronic Health Records and Care Coordination technology platform used by some of Massachusetts’ largest and most complex provider organizations. The company has over 15 years of experience providing EHR technology specifically to Massachusetts-based Outpatient and ESP/MCI programs.
In addition to EHR technology used in over 900 sites statewide, eHana provides the core Care Coordination technology powering 23 of the 27 MassHealth Community Partners (BH & LTSS), demonstrating its extensive success working with the Massachusetts Medicaid provider community, Accountable Care Organizations, and MassHealth. To date, eHana has transmitted over two million fully automated zero-paid claims for CP services.
eHana’s technology enables an integrated record to be shared seamlessly across core CBHC services, including CBHC Outpatient, MCI/ESP, and CCS. eHana’s success with similar multi-program modules includes youth Community Service Agency (CSA) programs, which operate as a coordinating entity for services such as In-Home Therapy, Intensive Care Coordination, and Therapeutic Mentoring.
eHana’s platform serves over 10,000 monthly active users in Massachusetts alone, writing over 600,000 documents per month on over 250,000 patient enrollments. The web-based system is widely regarded as being extremely clinician-friendly, and includes tools such as notifications and messaging to specifically enable cross program collaboration and coordination (e.g. between CBHC, MCI, and CCS).
Dedicated to Massachusetts Providers
eHana has been “at the table” with its providers for many of the most consequential statewide initiatives of the past 15 years, working closely with EOHHS, MassHealth, DMH, DDS, DPH, DCF, EIM, and many others to build innovative solutions to complex care and regulatory challenges faced by Massachusetts providers. While several of its customers provide services outside of the Commonwealth, eHana’s overriding focus is the Massachusetts market.
The company has invested significant resources into building robust integrations with Massachusetts state agencies, payers, and other stakeholders, including work with EVS, EIM/ESM, EOHHS SFTP, CANS, Virtual Gateway, Mass HIway, all MassHealth ACOs, PatientPing/Bamboo Health, Collective Medical Technologies/PointClickCare, and more. Most recently, eHana has partnered with a MassHealth ACO to implement automated Care Plan data exchange and PCP approval.
Over the past 15 years eHana has implemented systems across a wide variety of practice disciplines, including but not limited to Outpatient, SUD/Addiction, ESP/MCI, CCS, CBHI/CSA/IHT/TM/ICC, I/DD services, Residential Services, Community-Based Programs, Justice-Involved Services, Elder Services, Housing & Homelessness.
Innovative and Adaptable
Through its work with CP and other programs, eHana has extensive experience adapting its core technology to meet specific Massachusetts needs, including zero-paid and bundled claims logic, unique regulatory requirements such as the Massachusetts Medication Administration Program (MAP), and state-specific exports and reports (including automated submission and tracking of Massachusetts CANS submissions).
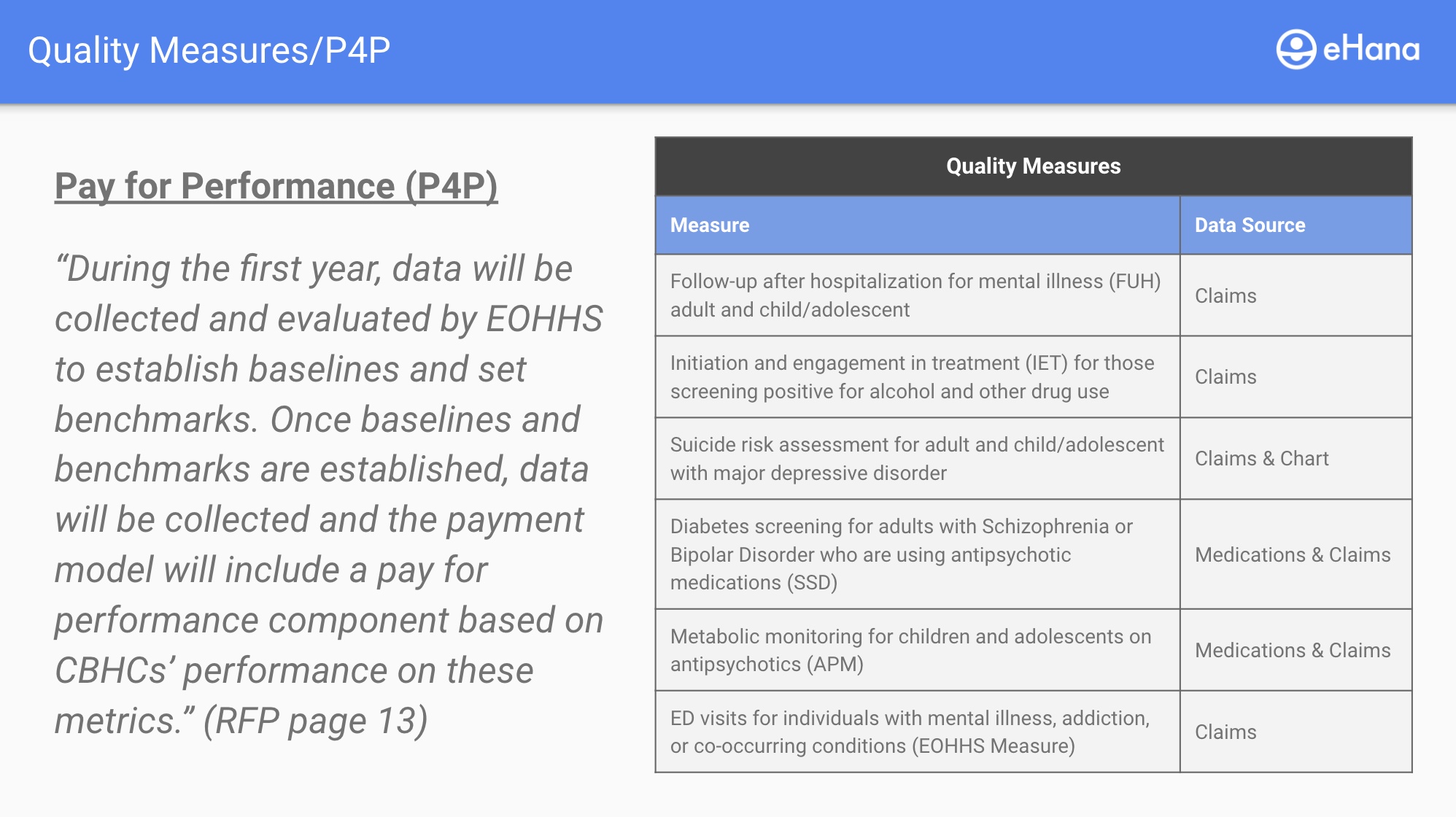
eHana’s reporting, data analytics, and replication solutions offer insight into core operational and quality metrics, including leveraging all-payer and MassHealth claims datasets to support whole-member quality measures and insights.
eHana’s core technology platform also enables integrated e-prescribing (including PDMP and controlled substances) and electronic integration with local Massachusetts-based laboratories. The platform supports integrations with additional third parties via its innovative “Sidecar” functionality.
Supporting Zero-Paid and Bundled Claims (XIII.F.5)
Organizations will use eHana’s HIT platform to transmit CBHC claims, both zero-paid and bundled. eHana’s platform supports such a configuration. By way of example, eHana has transmitted over two million zero-paid claims for the MassHealth Community Partner program since its inception.
CBHC billing workflow:
The eHana EHR, prior to services being rendered, will confirm via the Eligibility Verification System (EVS) that an individual client is eligible for the CBHC bundle rate
Users will document services as normal within the eHana EHR, indicating the date/time, service type, location, program code, and any applicable modifiers
If a client is eligible for the bundle rate, and a bundle-eligible service is entered, the resulting “charge” will be created with a zero rate
When the services for a given billable period are batched (daily, weekly, monthly, or ad hoc), the system will identify any days in the period in which a zero-paid, bundle-eligible charge exists and create a single corresponding bundle claim for that same day.
Both the zero-paid claims and the bundle claims will be included in the batch and are transmitted to the payer
Relevant vendor experience:
eHana’s existing EVS integration includes Massachusetts-specific functionality for flagging payers and plans sufficient to identify CBHC-eligible individuals
eHana has transmitted over two million zero-paid claims for the MassHealth Community Partner program
eHana has worked closely with the Massachusetts Department of Mental Health and its partners to implement daily electronic billing for Adult Community Clinical Services (ACCS), a process that involves examining services documented on a given calendar day and issuing a corresponding day-rate claim